Results
monitoring
At East Bay Behavior Therapy Center (EBBTC), a key aspect of our treatment approach is the use of standardized measurements and progress tracking for each client we work with.
Your mental health check-ins play a crucial role in our work together. We’ll measure your progress in ways that matter to you.
By consistently tracking your progress, we can tailor our interventions to your unique needs, goals and personal values, ensuring that your treatment remains focused and impacts your life.
These check-ins help you and your therapist or coach collaboratively plan your course of skills you need to achieve your goals.
By understanding what’s working (and what’s not), we can fine-tune your skills to fit your mental health needs perfectly.
If something’s not quite right, we’ll spot it together and make adjustments before it becomes a struggle in your life and our work together.
This data-driven approach provides tangible evidence of your progress over time.
By engaging in these regular check-ins at EBBTC you’re actively shaping your treatment, you’re not just participating in it.
How to complete a mental health check-in
tracking progress
At the end of each month, all clients are asked to complete the Depression, Stress, and Anxiety Scale (DASS) questionnaire, which is a standardized, clinically validated assessment of anxiety, stress, and depression.
In addition, we will ask you to complete other questionnaires focused on the quality of your life and what you’re working on in therapy.
Meaning of results: The results of your check-ins serve as a roadmap for your treatment. They help identify patterns in your emotional responses, enable the development of proactive strategies, and allow for timely adjustments to your sessions plan.
After every mental health check-in, you’ll be able to see your results and see a snapshot of what might have changed since your last session.
Your progress
tracking progress
The results of your check-ins serve as a roadmap for your treatment.
You’ll be able to see your results and a snapshot of what might have changed per month and then, making any necessary adjustments in your therapy sessions.
We use process and outcome measurements such as:
- Acceptance and Action Questionnaire
- Depression, Stress and Anxiety Scale
- Liebowitz Social Anxiety Scale
- Perfectionism Frost Scale
- Panic Severity Scale
- Penn Worry Questionnaire
- General Procrastination Scal
- Trauma Symptom Checklist
- Yale-Brown Obsessive Compulsive Scale
Case samples
client’s experiences
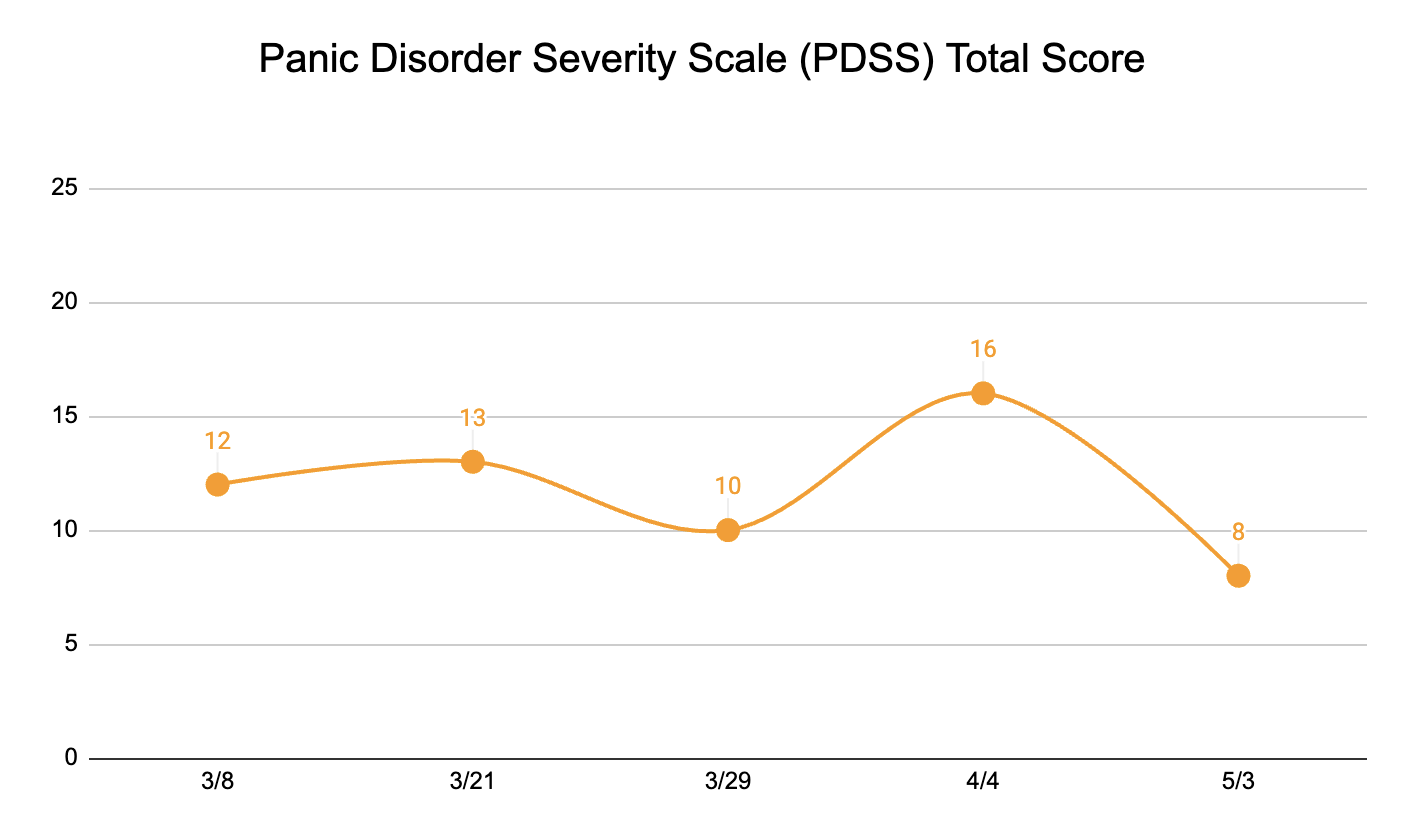
38-year old client with sudden panic attacks and fears of medical illnesses – ranging from heart arrhythmias to autoimmune diseases, – despite doctors denying any medical condition.
It begins with a racing heart, pounding so hard client can feel it in the throat, shortness of breathe, becomes short and quick, as if he can’t get enough air, a wave of dizziness, cold sweat breaks out across his forehead, and tingling sensations in the finger and toes.
Thoughts include, “Am I having a heart attack? Am I going to pass out? What if I can’t breathe?” These fears loop endlessly in her mind, each one feeding into the next.
Triggers included a “heart palpitation”, chest pain, and abdominal pain out of the normal.
Monitoring of treatment
Panic Disorder Severity Scale
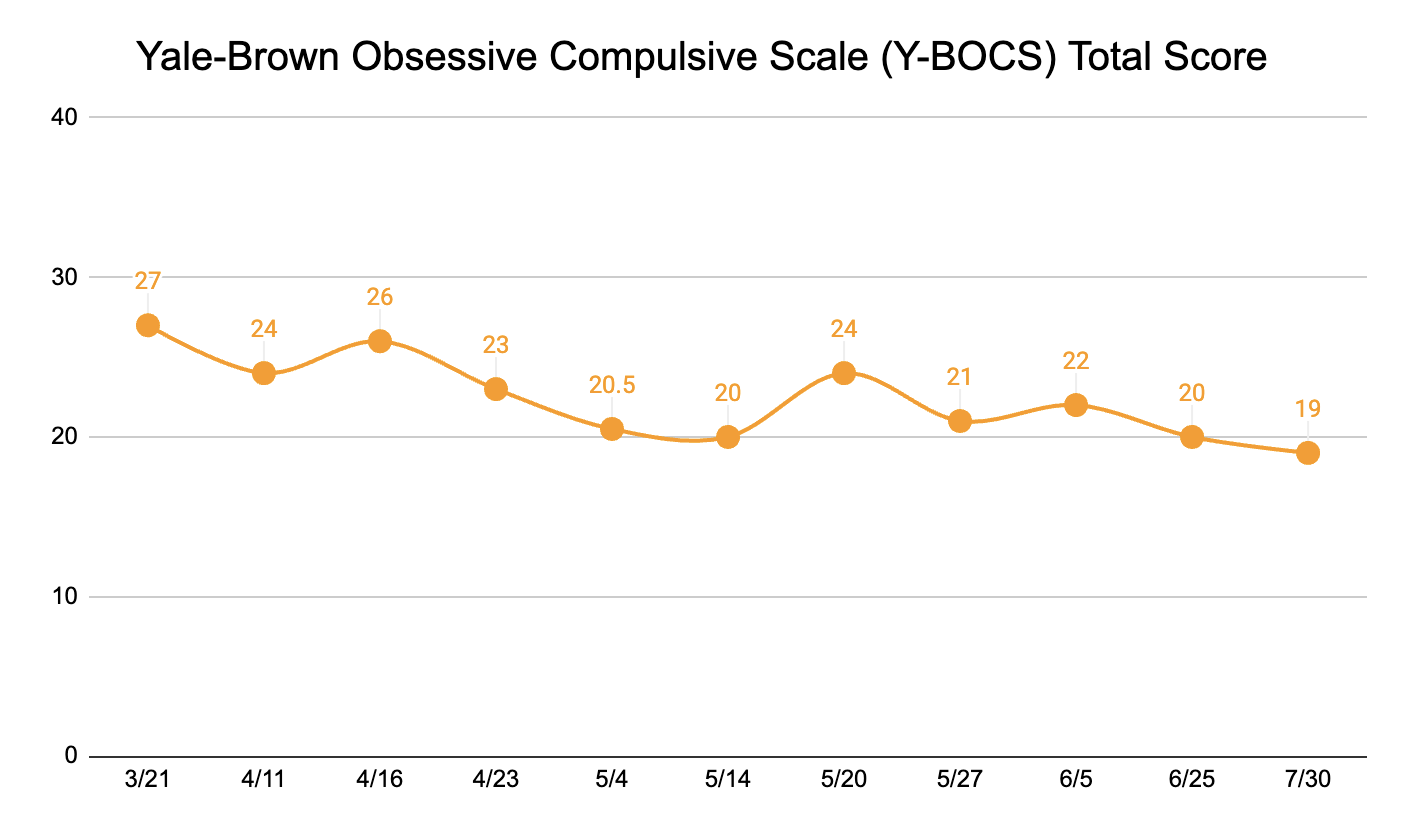
29-year old client struggling with obsessions related to death, telling the truth, contamination and superstitious thinking.
Compulsions included using gloves, doing things three times, opening door with foot or elbow, typing in a certain way to avoid contaminating laptop.
Mental compulsions included mentally figuring it out – did it touch part of my body/face that is contaminated ?, ruminating about death.
Monitoring of treatment
Yale-Brown Obsessive Compulsive Scale
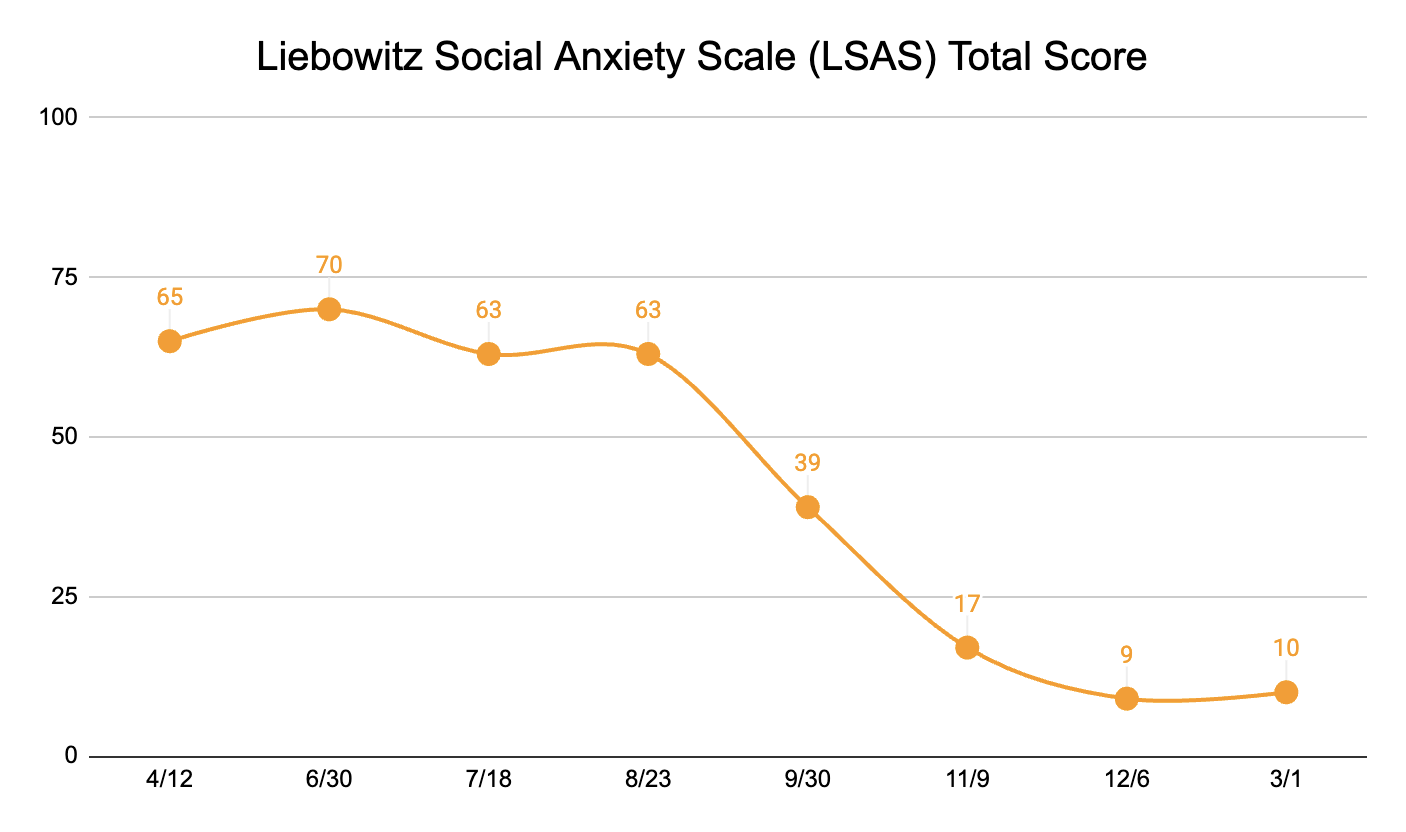
14-year old client struggling with social anxiety.
Client reported experiencing fear and avoiding the following situations: telephoning in public, eating in public, giving a talk in front of an office, writing while being observed, calling someone they don’t know, talking with people they don’t know, meeting strangers, using a public bathroom, entering a room where others are seated, expressing disagreement, eye contact, returning goods to a store, and throwing a party.
Monitoring of treatment
Liebowitz Social Anxiety Scale
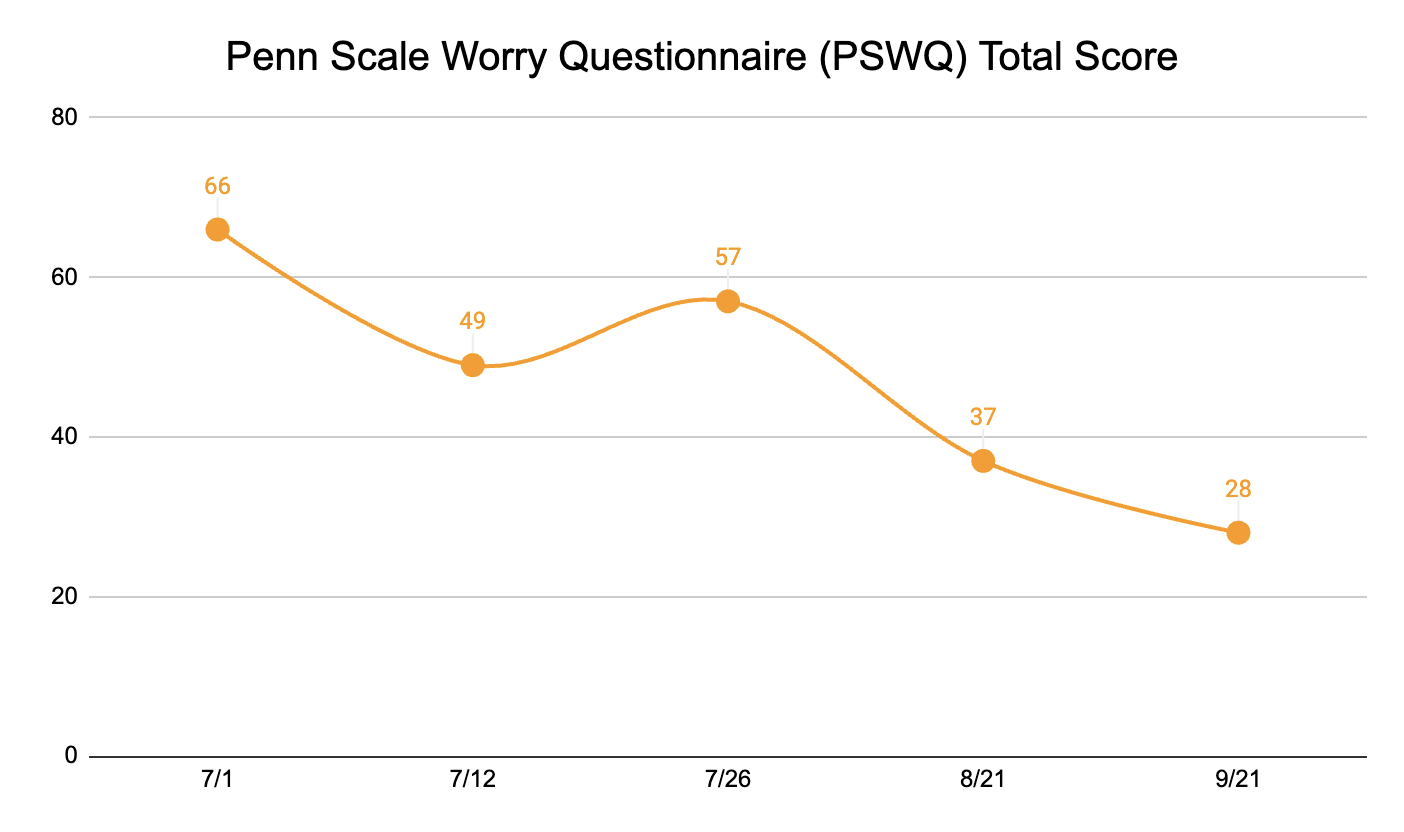
41-year old client suffering from chronic worry
Client’s mind raced with an endless stream of “what-if” scenarios as she lay awake at night, her heart pounding. Financial worries consumed her thoughts: “What if I lose my job? What if I can’t pay my rent next month? What if I never save enough for retirement?”
Client’s relationship with partner was another source of constant anxiety. “What if he’s losing interest in me? What if we argue and can’t resolve it? What if he meets someone else?”
Health concerns were also present. Every twinge or ache sent her spiraling: “What if this headache is actually a brain tumor? What if that mole is cancerous? What if I have an undiagnosed heart condition?” Client found herself constantly checking her body for signs of illness.
At work, client struggled with worry thoughts such as “What if I make a mistake on this important project? What if my presentation goes terribly? What if my boss is secretly dissatisfied with my work?”
Measurement
Penn Scale Worry Questionnaire
37-year old client suffering with social anxiety.
Client endorsed the following fears: telephoning in public, eating in public, working while being observed, writing while being observed, talking with people I don’t know very well, meeting strangers, urinating in a public bathroom, talking to people in authority, entering a room where others are already seated, speaking up in a meeting, taking a test, and expressing disagreement.
Monitoring of treatment
Liebowitz Social Anxiety Scale

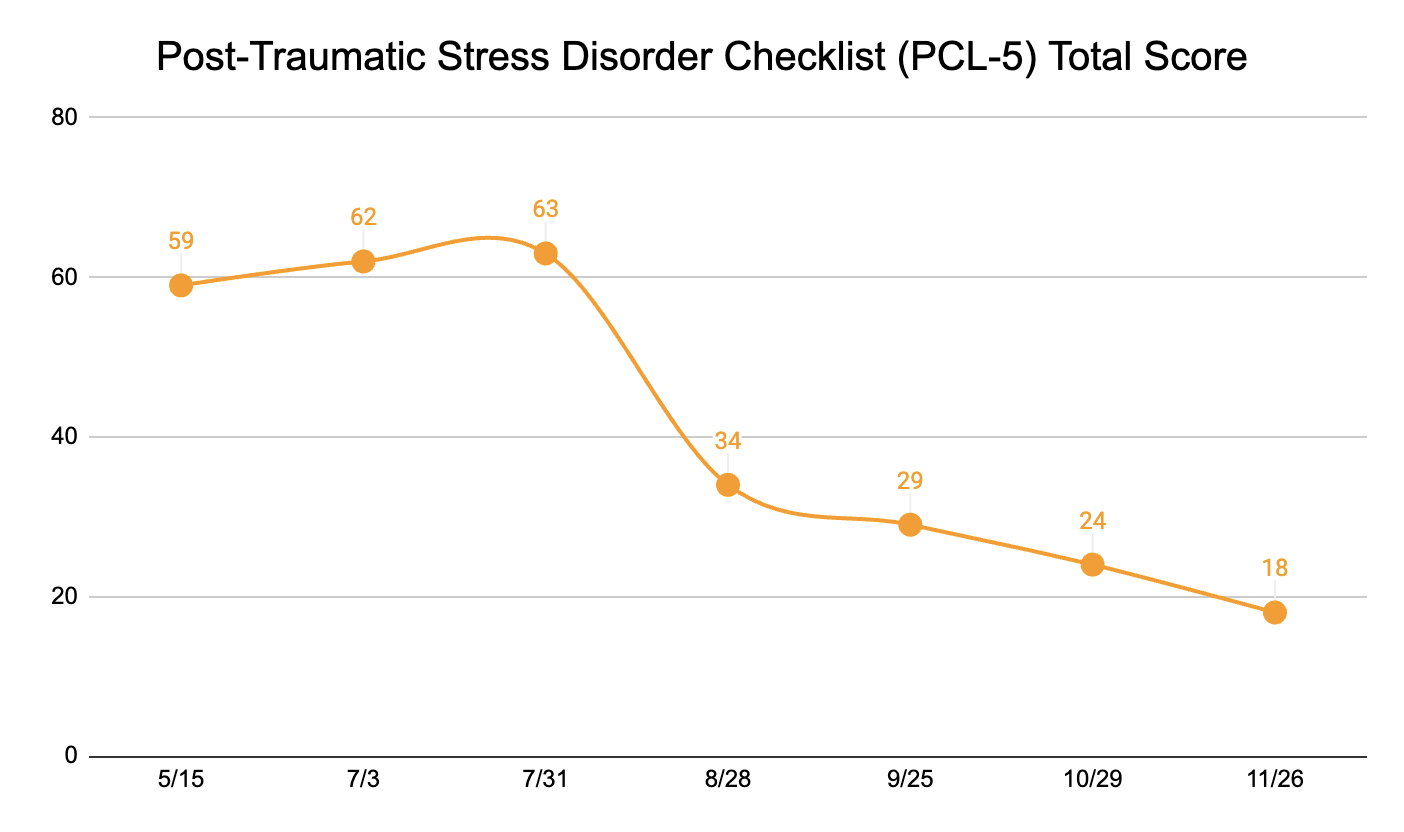
51-year-old client suffering from Post-Traumatic Stress Disorder.
Client often finds himself reliving the traumatic event through vivid, unwanted memories that intrude on his thoughts during the day.
His body seemed to be in a constant state of high alert; he startled easily at unexpected noises and felt tense and on edge most of the time. He had difficulty concentrating on tasks at work and home, and his mind often felt foggy.
To cope with these overwhelming feelings, client stopped going to places or engaging in activities he once enjoyed because they triggered painful memories. Client has also withdrawn from friends and family, finding it difficult to connect emotionally or talk about his experiences. Client often felt numb and disconnected from his surroundings, as if he was watching his life from a distance.
Client felt stuck and unsure how to move forward.
Monitoring of treatment
Post-Traumatic Stress Disorder Checklist 5
Online courses
Home-study programs
You can learn actionable, compassionate and research-based skills from the comfort of your own home and at your pace.
Each online class includes high-quality videos, worksheets, and audio-recorded exercises.

LEARN MORE
LEARN MORE
LEARN MORE
LEARN MORE
LEARN MORE

LEAN MORE
Why our clients love working with us
testimonials
How to start working with us
get unstuck
Figure out what's really keeping you stuck and struggling by having a comprehensive intake session.
We work with children, teens, and adults and do our best to get you back into your life!